Fill a Valid Tb Test Template
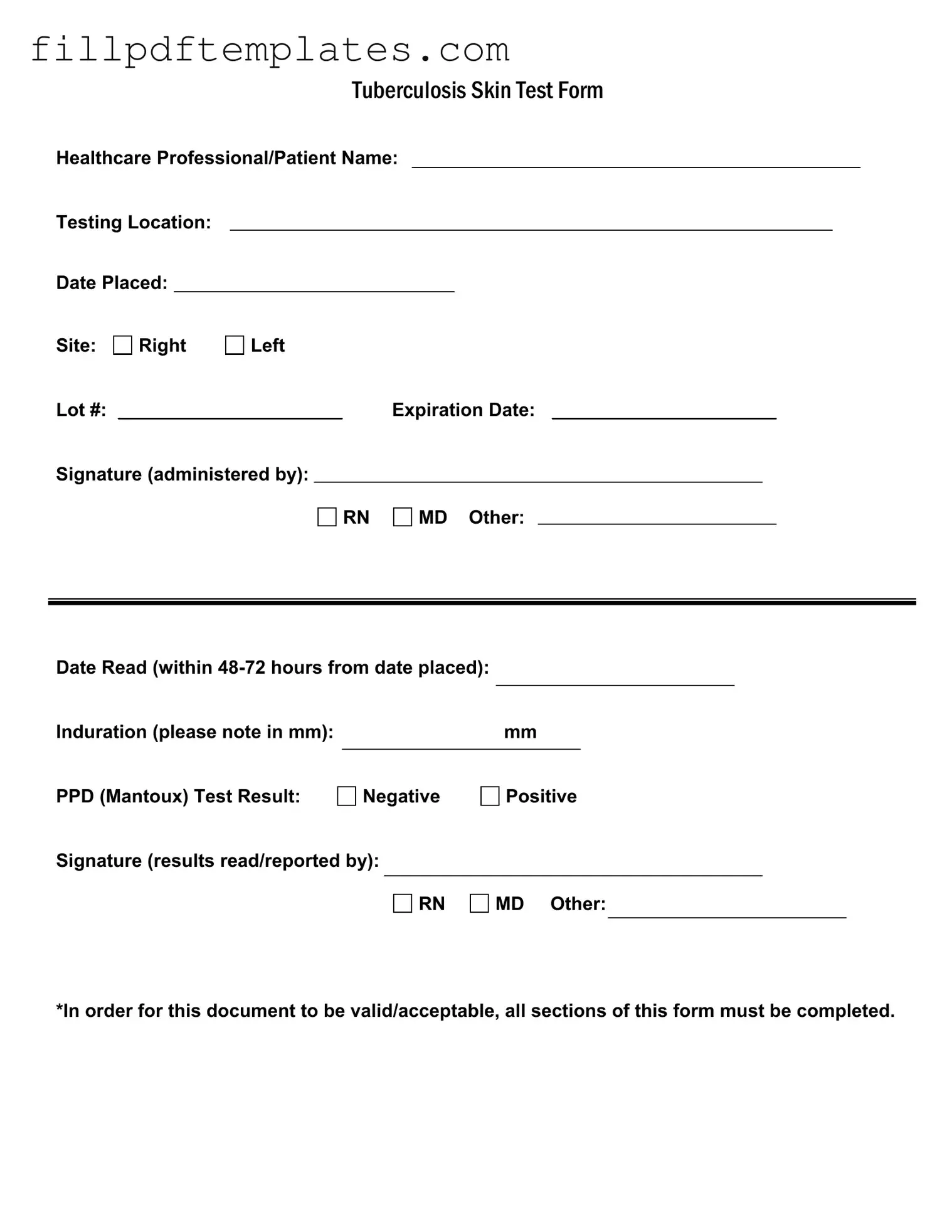
The Tuberculosis (TB) Skin Test Form is an essential document used in the healthcare setting to record important information regarding TB testing. It includes key details such as the names of the healthcare professional and patient, as well as the testing location and the date the test was placed. The form requires specific information about the site of the test, whether it was administered on the right or left side, and includes a lot number along with its expiration date. A signature from the administering professional—be it a registered nurse (RN), medical doctor (MD), or another qualified individual—is also necessary to validate the test. After the test is placed, it is crucial to read the results within 48 to 72 hours, noting the induration in millimeters to determine the test outcome. The final result, whether negative or positive, must be clearly indicated, along with the signature of the professional who read and reported the results. To ensure the document is valid and acceptable, it is imperative that all sections of this form are completed accurately.
Additional PDF Templates
Horse Training Agreement Template - The Owner must disclose any dangerous behaviors or conditions of the horse prior to training.
For more information and to access the necessary documentation, visit arizonaformpdf.com/, which provides helpful templates and resources related to the Notice to Quit form and the eviction process in Arizona.
Progressive Virtual Inspection - Understand which services are necessary versus optional for your vehicle.
A305 Form - This form is standardized by the American Institute of Architects.
Similar forms
- Vaccination Record: Similar to the TB Test form, a vaccination record documents immunizations received by an individual. It includes details such as the type of vaccine, administration date, and healthcare provider's signature.
- Medical History Form: This form collects comprehensive health information from patients. Like the TB Test form, it requires personal details and is often completed before medical appointments.
- Consent for Treatment Form: This document outlines the patient's consent for medical procedures. It shares the need for signatures and dates, ensuring all information is accurately recorded.
- Patient Registration Form: This form gathers essential personal and insurance information. It is similar in that it must be filled out completely for the patient's file to be valid.
- Health Screening Questionnaire: Used to assess an individual's health status, this questionnaire often requires specific details about symptoms or conditions, much like the TB Test form.
- Release of Information Form: This document allows healthcare providers to share a patient’s medical records. It necessitates signatures and can only be valid if all required sections are filled out.
- Referral Form: This form is used to refer a patient to a specialist. It includes patient details and the reason for the referral, similar to the structured format of the TB Test form.
Hold Harmless Agreement: This document is essential for any parties entering into a transaction that involves potential legal risks. It ensures that one party will not hold the other liable for any damages or injuries that may occur, making it crucial for risk management. For more details, refer to the Hold Harmless Agreement.
- Prescription Pad: A healthcare provider uses this pad to prescribe medications. Like the TB Test form, it requires clear information about the patient and must be signed by the provider.
- Emergency Contact Form: This document lists individuals to contact in case of an emergency. It shares the requirement for complete and accurate information to ensure effectiveness.
- Patient Follow-Up Form: This form tracks a patient’s progress after treatment. It includes sections for notes and results, similar to the TB Test form's focus on documenting outcomes.
Document Specifics
| Fact Name | Details |
|---|---|
| Form Title | Tuberculosis Skin Test Form |
| Required Information | All sections of the form must be completed for validity. |
| Testing Method | PPD (Mantoux) test is the method used for screening. |
| Reading Timeframe | The test must be read within 48-72 hours after placement. |
| Result Options | Results can be either Negative or Positive. |
| Signature Requirement | Results must be signed off by a healthcare professional (RN, MD, or other). |
Things You Should Know About This Form
-
What is a TB Test Form?
The TB Test Form is a document used to record the administration and results of a tuberculosis skin test, commonly known as the PPD or Mantoux test. It captures essential details such as patient information, testing location, and the results of the test.
-
Who needs to fill out the TB Test Form?
Healthcare professionals who administer the TB test must complete the form. Additionally, patients receiving the test should ensure their personal information is accurately recorded. This form is crucial for tracking and managing tuberculosis screenings.
-
What information is required on the TB Test Form?
The form requires several key pieces of information:
- Healthcare Professional/Patient Name
- Testing Location
- Date Placed
- Site of the test (Right or Left)
- Lot number and expiration date of the test
- Signature of the administering professional
- Date Read (within 48-72 hours)
- Induration measurement in mm
- PPD Test Result (Negative or Positive)
- Signature of the person reading the results
-
What does the Induration measurement indicate?
Induration refers to the raised, hardened area that forms at the test site. The size of this area, measured in millimeters (mm), helps determine whether the test result is positive or negative. A larger induration typically indicates a positive result, suggesting potential exposure to tuberculosis.
-
How soon should the test results be read?
The results of the TB test should be read within 48-72 hours from the date the test was placed. It is essential to adhere to this timeframe to ensure accurate interpretation of the results.
-
What happens if the form is incomplete?
For the TB Test Form to be valid, all sections must be completed. An incomplete form may lead to delays in processing or result reporting, and it could affect the patient's medical record and subsequent care.
-
What should I do if I receive a positive test result?
If you receive a positive result, it is important to follow up with your healthcare provider. They may recommend further testing, such as a chest X-ray or sputum test, to determine if you have active tuberculosis. Early intervention is crucial for effective treatment.
-
Is the TB Test Form necessary for employment or school requirements?
Yes, many employers and educational institutions require proof of a negative TB test as part of their health screening process. The completed TB Test Form serves as official documentation of your test results and is often requested during the application or enrollment process.
Documents used along the form
When dealing with tuberculosis testing, several other forms and documents often accompany the TB Test form. Each of these documents serves a specific purpose, ensuring that the testing process is thorough and compliant with health regulations. Below is a list of common forms you might encounter.
- Medical History Form: This document collects information about the patient's past health issues, medications, and any previous TB tests. It helps healthcare providers assess risk factors.
- Informed Consent Form: Patients must understand the procedure and its implications. This form ensures that they are informed and agree to the TB test.
- Last Will and Testament Form: For those planning their estate, consult the essential guidelines for Last Will and Testament preparation to ensure all wishes are accurately documented.
- TB Symptom Questionnaire: This form lists common TB symptoms, allowing healthcare professionals to evaluate whether further testing is necessary based on the patient's current health status.
- Release of Information Form: If results need to be shared with other healthcare providers or institutions, this form grants permission for the release of medical records.
- Follow-Up Appointment Schedule: After the TB test, patients may need to schedule a follow-up appointment. This document outlines the next steps and ensures continuity of care.
- Results Notification Form: This form communicates the results of the TB test to the patient. It often includes information on what the results mean and any necessary actions.
- Referral Form: If a patient tests positive, a referral form may be used to connect them with specialists for further evaluation and treatment.
These documents are essential for ensuring a comprehensive approach to tuberculosis testing and management. They help streamline communication and maintain accurate records, ultimately supporting better patient care.
Tb Test Preview
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.