Fill a Valid Progress Notes Template
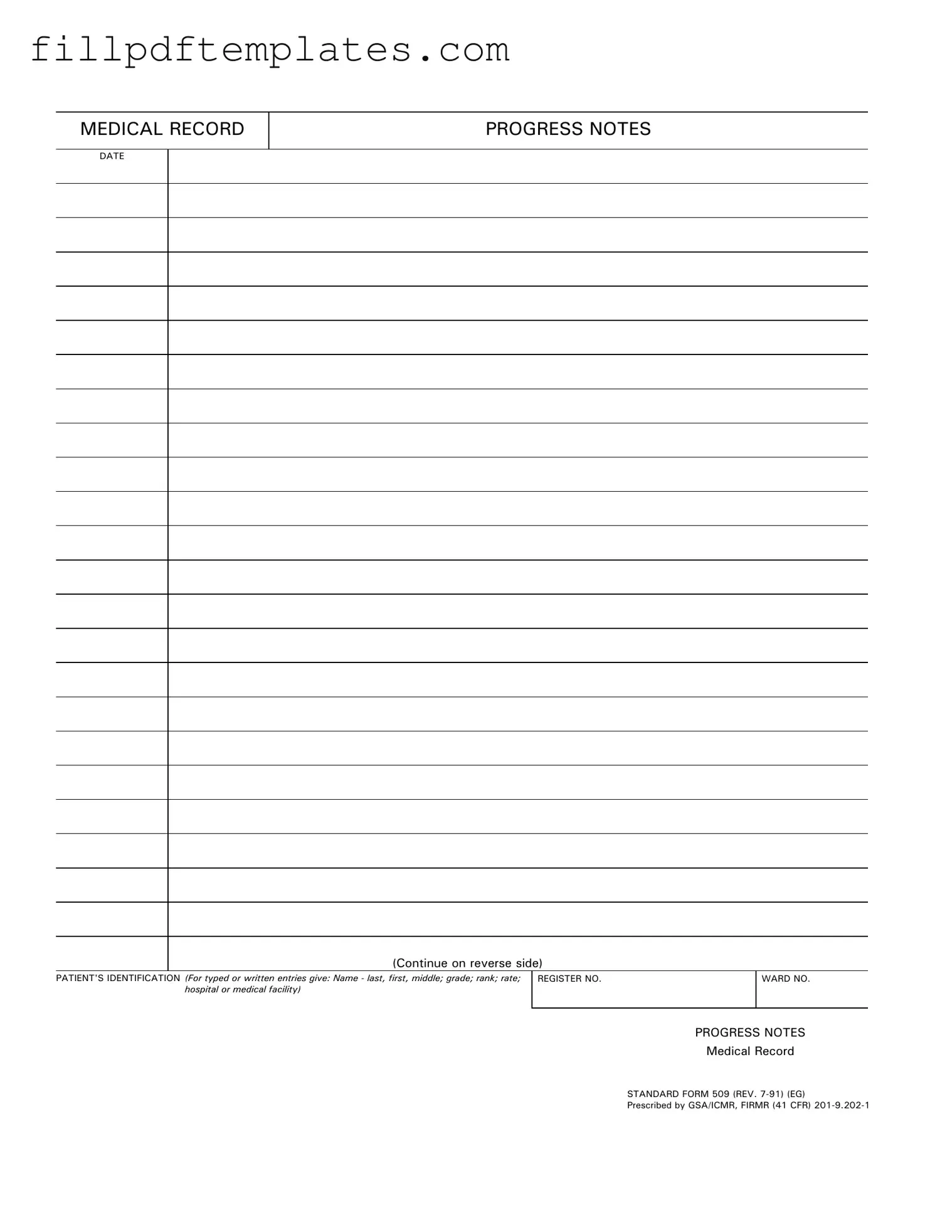
In the realm of healthcare, effective communication and documentation are paramount, and the Progress Notes form serves as a vital tool in this process. This standardized document, known as Standard Form 509, is designed to capture essential information about a patient's care and treatment over time. It includes critical details such as the patient's identification, which encompasses their name, grade, rank, and the medical facility where they are receiving care. Additionally, the form requires the date of each entry, ensuring that the timeline of a patient's progress is clear and organized. By using this form, healthcare providers can document observations, treatment plans, and any changes in a patient's condition, creating a comprehensive record that is essential for ongoing care. The structure of the Progress Notes form not only facilitates easy access to patient information but also adheres to regulatory standards, promoting consistency and accuracy in medical records. As healthcare professionals navigate the complexities of patient care, the Progress Notes form stands as a cornerstone of effective medical documentation.
Additional PDF Templates
Tenancy Agreement Addendum - Details on utility payments ensure that there are no misunderstandings regarding who is responsible for these expenses.
Dr-835 - Make sure to accurately fill out the Tax POA DR 835 to avoid complications.
The District of Columbia Transfer-on-Death Deed form allows property owners to designate beneficiaries who will receive their real estate upon their passing, without the need for probate. This form provides a straightforward way to transfer property, ensuring that the owner's wishes are honored while simplifying the process for heirs. For more information, visit todform.com/blank-district-of-columbia-transfer-on-death-deed/ to get started on securing your property transfer.
Waiver of Lein - The waiver is specifically used within the state of Illinois for legal clarity.
Similar forms
The Progress Notes form serves a vital role in documenting patient care within medical records. Several other documents share similarities with the Progress Notes form in terms of purpose and structure. Below are four such documents:
- Patient Encounter Form: This document records the details of a patient visit, including symptoms, diagnosis, and treatment. Like Progress Notes, it provides a comprehensive overview of the patient’s condition and the care provided during the encounter.
-
Medical Power of Attorney: This essential document ensures that your healthcare decisions are made by someone you trust when you are unable to do so yourself. To learn more about the Arizona Medical Power of Attorney form, you can visit https://arizonaformpdf.com.
- SOAP Notes: SOAP stands for Subjective, Objective, Assessment, and Plan. This format organizes patient information systematically. Both SOAP Notes and Progress Notes aim to capture ongoing patient care and facilitate communication among healthcare providers.
- Discharge Summary: This document summarizes a patient's hospitalization and outlines follow-up care. Similar to Progress Notes, it reflects the patient’s progress and outcomes, serving as a critical tool for continuity of care.
- Clinical Pathway Document: This outlines the expected course of treatment for specific conditions. Both documents provide a framework for patient care, ensuring that all necessary steps are documented and followed throughout the treatment process.
Document Specifics
| Fact Name | Description |
|---|---|
| Form Title | The form is officially titled "Medical Record Progress Notes." |
| Governing Laws | This form is prescribed by GSA/ICMR, FIRMR under 41 CFR 201-9.202-1. |
| Revision Date | The current version of the form was revised in July 1991. |
| Patient Identification | It requires detailed patient identification including name, grade, rank, and rate. |
| Register and Ward Numbers | Sections for register number and ward number are included for tracking purposes. |
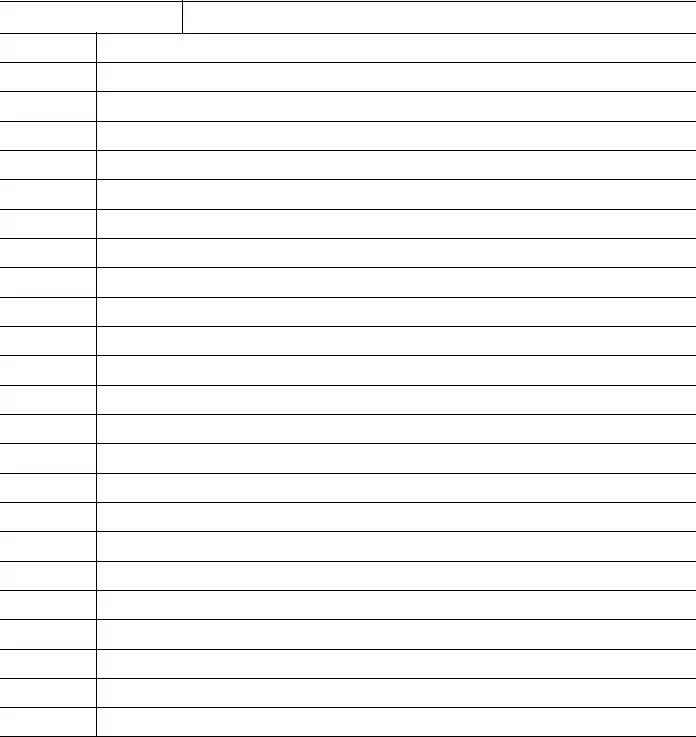
| Continuity | The form allows for continuation on the reverse side for additional notes. |
| Standard Form Number | The form is designated as Standard Form 509. |
| Usage Context | Primarily used in medical facilities for documenting patient progress. |
Things You Should Know About This Form
-
What is the purpose of the Progress Notes form?
The Progress Notes form is used to document a patient's medical history, treatment, and progress during their stay at a medical facility. It ensures that all relevant information is recorded systematically for future reference.
-
Who should fill out the Progress Notes form?
Healthcare providers, including doctors, nurses, and other medical staff, are responsible for completing the Progress Notes form. They must provide accurate and timely updates on the patient's condition and treatment.
-
What information is required on the Progress Notes form?
The form requires the patient's identification details, including their name (last, first, middle), grade, rank, rate, hospital or medical facility, as well as the date of entry. Additionally, it includes sections for documenting the patient's progress and any relevant observations.
-
How often should Progress Notes be updated?
Progress Notes should be updated regularly, ideally after each patient encounter or treatment session. This ensures that all changes in the patient's condition are recorded promptly and accurately.
-
Can the Progress Notes form be modified?
While the form itself should remain standardized to ensure consistency, healthcare providers may add notes or comments as necessary. However, any modifications to the official form should comply with institutional policies.
-
Is there a specific format to follow when filling out the Progress Notes?
Yes, it is important to follow the standard format outlined in the form. Entries should be clear and concise, using professional language. Avoid abbreviations that may not be universally understood.
-
What happens to the Progress Notes after they are completed?
Once completed, the Progress Notes become part of the patient's medical record. They are stored securely and can be accessed by authorized personnel for future reference, ensuring continuity of care.
-
How can I ensure the confidentiality of the Progress Notes?
To maintain confidentiality, only authorized personnel should have access to the Progress Notes. Additionally, ensure that the notes are stored in a secure location and that any electronic records are protected by appropriate security measures.
Documents used along the form
When managing patient care, several documents complement the Progress Notes form. Each of these documents plays a vital role in maintaining accurate and comprehensive medical records. Below is a list of commonly used forms that work alongside Progress Notes.
- Patient Intake Form: This document collects essential information about the patient, including personal details, medical history, and current medications. It serves as a foundation for future care.
- Treatment Plan: This outlines the proposed course of treatment for the patient. It includes goals, interventions, and timelines, ensuring everyone involved understands the patient's care strategy.
- Consent for Treatment: This form confirms that the patient has been informed about the treatment options and has agreed to proceed. It protects both the patient and the healthcare provider legally.
- Referral Form: When a patient needs to see a specialist, this document facilitates the referral process. It includes relevant medical information and the reason for the referral.
- Motor Vehicle Bill of Sale: For those in need of transferring vehicle ownership, our comprehensive Motor Vehicle Bill of Sale documentation ensures that all legal aspects are properly addressed.
- Discharge Summary: This document summarizes the patient's treatment, progress, and follow-up care upon discharge. It ensures continuity of care and provides important information to future healthcare providers.
- Medication Administration Record (MAR): This tracks all medications administered to the patient, including dosages and times. It helps prevent medication errors and ensures compliance with the treatment plan.
- Insurance Verification Form: This document confirms the patient's insurance coverage and benefits. It is essential for determining financial responsibility and ensuring that services are covered.
Utilizing these documents alongside the Progress Notes form enhances patient care and supports effective communication among healthcare providers. Each form contributes to a comprehensive understanding of the patient's health journey.
Progress Notes Preview
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.